Case 2 spleenomegaly
February 10, 2022
A 23 YEAR OLD MALE WITH MEGALOBLASTIC ANAEMIA SECONDARY TO VITAMIN B 12 DEFICIENCY ? ASYMPTOMATIC CELIAC DISEASE, FISSURE IN ANO.
UDHC SIMILAR CASES
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment"
A 23 year old male studied up to intermediate, currently working as driver came to OPD with
C/O yellowishdiscoloration of eyes since 15 days.
C /O fever since 1 week
SOB on extertion since 1 week
abdominal discomfort and pain since 1week
blood in stools 1 episode ,2 days back.
HOPI: patient was apparently asymptomatic 3 years back, history of fever went to hospital ,on examination PALLOR +, investigations :Hb-4 gm%,-3 PRBC transfusions done 3 years back, attenders said that his anaemia is secondary to B12 deficiency, patient received the B12 injections ,his Hb improved from 4 gm%to 12 gm% and also planned for bone marrow biopsy, but they didn't perform as he was improved with B12 injections.
After this episode, no similar complaints until 15 days back ,suddenly developed yellowish discoloration of eyes 15 days back, he was taken to a local RMP said to have jaundice, patient took herbal medication for 1 week.
Fever: high grade, associated with chills and rigor,SOB on exertion (Grade 2 )
SOB insidious inonset, gradually progressive from GRADE I to GRADE 2 in 1 week.
Orthopnea +, No PND.
PAIN ABDOMEN:squeezing type, intermittent associated with nausea.
Blood in stools
1 episode 2 days back, normal consistency. No vomitings,hemoptysis, ,hematemesis ,melena .
He is also complaining of burning sensation while passing stools since 2 days.
PAST H/0: H/o blood transfusion 3 yrs back.
PERSONAL H/O :Diet-mixed
Appetite -normal Sleep-adequate
Bowel &bladder movements-regular
ALCOHOL H/O: 1-2 beers for every 3 weeks.
DIET:
O/E : Pt is c/c/c
Bp- 100/60 mm Hg
PR-80 bpm
RR-20 cpm
Spo2-100%@ RA
Grbs-92 mg/dl
Pallor-++
Icterus-+ mild
No cyanosis, clubbing, no lymphadenopathy.
Oedema of feet -+ , upto B/L ankles.
Hyperpigmentation of knuckles:+
SE:CVS- S1, S2+, JVP raised
Flow murmur +,
Venous hump +
Apex beat :at 5th IC space.
RS: BAE+
P/A: mild hepatomegaly+
splenomegaly + 2cms below the coastal lime
BS +
CNS :NAD
PROVISIONAL DIAGNOSIS: PANCYTOPENIA UNDER EVALUATION? Secondary to Vitamin B12 deficiency.
CHEST X- RAY DONE ON :10/2/22
USG DONE OUTSIDE ON :7/2/22
2D ECHO DONE ON :10/2/22
ECG done on :10/2/22
USG DONE ON 10/2/22
Review USG done on 12-2-22
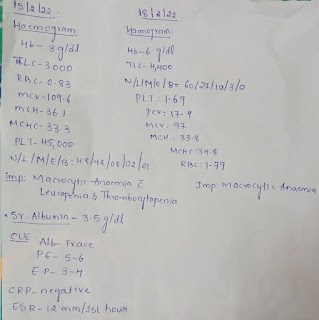
INVESTIGATIONS
Surgery opinion :done on 14/2/22
Investigations done on :15/2/22 &18/2/22.
ICU BED-3
DAY-1
S: sob subsided,pain abdomen subsided
O: BP:100/80 mmHg
PR:120 bpm
RR:18 cpm
SPO2: 99% at RA
GRBS: 93mg/dl
Stools: not passed
RS:BAE+
CVS: S1S2 +
P/A:Soft,non tender,bs+
CNS:NAD
I/O:500/200ml
A: Pancytopenia under evaluation secondary to ?B12 deficiency
P: Inj. Methylcobalamine 1500mcg in 100ml NS IV/OD
Inj. Lasix 20mg BD(8am—4pm—x)if SBP >110mmHg
Inj. Pantop 40mg IV/SOS
Inj. Zofer 4mg IV/SOS
Tab. Ultracet 1/2 PO/SOS
Tab. PCM 500mg PO/SOS
Monitor vitals 4th hourly
I/O,Temp charting
GRBS 12th hourly
1 unit of PRBC transfusion done on 10/2/22 , started at 11:30 PM, ended on 5AM 11/2/22.
ICU BED-3
DAY-2
S: No sob,pain abdomen,fever,bleeding manifestations
O: BP:100/50 mmHg
PR:108 bpm
RR:20 cpm
SPO2: 99% at RA
GRBS: 79mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,non tender,bs+
CNS:NAD
I/O:1200/950ml
Stools passed
A: Pancytopenia under evaluation secondary to ?B12 deficiency
P: Inj. Methylcobalamine 1500mcg in 100ml NS IV/OD(Day-2)
Inj. Pantop 40mg IV/SOS
Inj. Zofer 4mg IV/SOS
Tab. Ultracet 1/2 PO/SOS
Tab. PCM 500mg PO/SOS
Monitor vitals 4th hourly
I/O,Temp charting
GRBS 12th hourly
AMC BED-3
DAY-3
S: No sob,pain abdomen,fever,bleeding manifestations
O: BP:110/70 mmHg
PR:93 bpm
RR:20 cpm
SPO2: 99% at RA
GRBS: 75mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +,Splenomegaly + 1cm below left coastal margin
CNS:NAD
I/O:700/1250ml
Stools passed
A: Pancytopenia under evaluation secondary to ?B12 deficiency
P: Inj. Methylcobalamine 1500mcg in 100ml NS IV/OD(Day-3)
Inj. Pantop 40mg IV/SOS
Inj. Zofer 4mg IV/SOS
Tab. Ultracet 1/2 PO/SOS
Tab. PCM 500mg PO/SOS
Monitor vitals 4th hourly
I/O,Temp charting
GRBS 12th hourly
AMC
BED NO :3
DAY-4
S: No sob,pain abdomen,fever
1 episode of blood in stools yesterday
O: BP:110/60 mmHg
PR:92 bpm
RR:20 cpm
SPO2: 99% at RA
GRBS: 78mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +
CNS:NAD
I/O:850/1600ml
Stools passed
A: Pancytopenia under evaluation secondary to ?B12 deficiency
P: Inj. Methylcobalamine 1500mcg in 100ml NS IV/OD(Day-4)
Tab. PCM 500mg PO/SOS
Monitor vitals 8thhourly
I/O,Temp charting
GRBS 12th hourly
..................
Ward updates:23yr/M
DAY-5
S: No sob,pain abdomen,fever, no blood in stools, thrombophlebitis present, edema of eyelids present, and face present
O: BP:100/80 mmHg
PR:85 bpm
RR:20 cpm
SPO2: 99% at RA
GRBS: 78mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +,
CNS:NAD
Stools passed
A: Pancytopenia under evaluation secondary to ?B12 deficiency
P: Inj. Methylcobalamine 1000mcg in 100ml NS IV/OD+0.75 mg FA(Day-5)
Tab. PCM 500mg PO/SOS
High fibre diet +adequate hydration
Sitz bath for 20 min /TID
ointment lignocaine for LA/BD
Tab. OXERUTE OD X 2 days
Monitor vitals 4th hourly
I/O,Temp charting
GRBS 12th hourly
Haemogram :13/2/22
Hb-3. 2 g/dl
TLC-4, 400
N/L/E/M/B:35/55/03/07/00
PCV-8. 9
MCH-35. 1
MCHC-35. 3
RDW-32. 6
PLT-35, 000
RBC-0. 90 millions/cumm
General medicineward case
DAY-6
S: No sob,pain abdomen, 1 episode of fever spike at 8 AM.
No episode of blood in stool yesterday,no thrombophlebitis , edema of right side of face present
O: BP:100/60 mmHg
PR:88bpm
RR:20 cpm
SPO2: 99% at RA
GRBS: 78mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +,
CNS:NAD
Stools passed yesterday
A: megaloblastic anemia secondary to B12 defiecency
P: Inj. Methylcobalamine 1500mcg in 100ml NS IV/OD + 0.75 mg FA(Day-6)
Tab pcm 500 mg po/soa
High fiber diet + adequate hydration
Sitz bath for 20 min/ tid
Ointment lignocaine for LA /BD
Tab OXERUTE X 2 DAYS
.................
Ward case :Day 7 updates:
S: No fever spikes, edema of right side of face decreased.
O: BP:100/70 mmHg
PR:88bpm
RR:19cpm
SPO2: 99% at RA
GRBS: 78mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +,
CNS:NAD
Stools passed
A: Megaloblastic anemia secondary to VitB12 deficiency ? Asymptomatic celiac disease
P: Inj. Vitcofol 1500microgm im/od.
Tab pcm 500 mg po/sos.
Tab Pantop 40mg po/od
High fiber diet + adequate hydration with gluten free diet
Sitz bath for 20 min/ tid
Ointment lignocaine for LA /BD
...................
General medicineward case
DAY-8
S: No fever spikes, edema of right side of face decreased.
O: BP:100/70 mmHg
PR:82bpm
RR:19cpm
SPO2: 98% at RA
GRBS: 86mg/dl
RS:BAE+
CVS: S1S2 +
P/A:Soft,bs +,
CNS:NAD
Stools passed
A: Megaloblastic anemia secondary to VitB12 deficiency ? Asymptomatic celiac disease fissure in ano
P: Inj. Vitcofol 1500microgm im/od.(weekly once)
Tab pcm 500 mg po/sos.
Tab Pantop 40mg po/od
High fiber diet + adequate hydration with gluten free diet
Sitz bath for 20 min/ tid (after defecation)
Ointment lignocaine for LA /BD (before defecation).
Bone marrow aspiration and biopsy done reports awiated
BONE MARROW BIOPSY

.jpg)

















Comments
Post a Comment